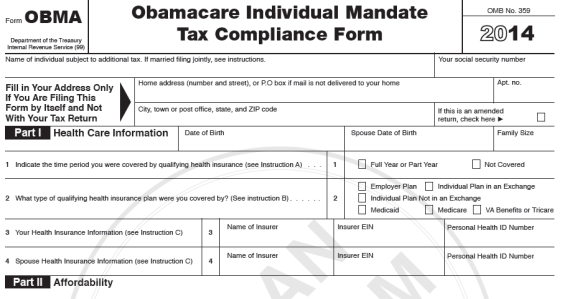
A conservative group misleads taxpayers on the Affordable Care Act and the Internal Revenue Service’s future role in enforcing it. Americans for Tax Reform posted a “projected” IRS tax form on its website that claims to “help families and tax specialists prepare” for new tax provisions under the health care law. But ATR makes several false claims:
- The group claims taxpayers will have to disclose “personal identifying health information” to the IRS to prove they have insurance. It quotes an IRS official who said taxpayers will report their “insurance information.” But the official also said the agency will not collect “any personal health information.”
- ATR says employers must offer preventative coverage that includes “abortion and hair loss treatment.” That’s not true. The law requires smaller insurance plans to cover preventative services, but states decide if those services include abortion. Even then, each state must have at least one plan that does not cover abortion.
- The group says failing to comply with the law could result in “interest against your property.” The law specifically bans the IRS from filing liens and levies against persons who fail to pay the tax for lacking insurance.
- ATR claims taxpayers can apply for a waiver from the health care law. That’s false. The government has given temporary waivers to some companies — not taxpayers — regarding one provision of the law, which involves benefit caps.
ATR says it created the tax form — just days before the presidential election — as a “service to the public.” Our public service is to correct the record.
Not Getting Personal
Starting in 2014, the health care law requires most Americans to have insurance or pay a tax, although exemptions will apply based on income and other factors. The IRS will require most taxpayers to prove they’re covered or they must pay a tax on their 2014 tax returns.
The IRS hasn’t issued exact procedures for how taxpayers will prove they have insurance. But that hasn’t stopped ATR from making misleading statements.
In an introduction to the tax form and in the instructions, ATR claims the IRS will require Americans to disclose:
- “Personal identifying health information”
- “The nature of their health insurance”
- “Insurance card information”
ATR bases its claim on a snippet of congressional testimony from then-IRS deputy commissioner Steven Miller in September. ATR quotes from Miller’s prepared remarks, in which he stated that “taxpayers will file their tax returns reporting their health insurance coverage and/or making a payment.”
But Miller explicitly stated that the IRS will not collect “any personal health information.”
Miller, Sept. 11: Taxpayers will get a form at the end of every year from their insurer to use when they prepare their tax returns. It is important to note that the information that insurers provide to the IRS will show the fact of insurance coverage, and will not include any personal health information.
In most cases, taxpayers will file their tax returns reporting their health insurance coverage, and/or making a payment, and there will be no need for further interactions with the IRS.
Douglas Shulman, who recently stepped down as IRS commissioner, also addressed privacy concerns. He told Congress in August that the IRS will verify whether or not a taxpayer has insurance. But he said the agency will not ask for personal information (See part 2, minute 40:00).
U.S. Rep. Danny K. Davis, Aug. 2: There are also individuals who … claim that the Internal Revenue Service is going to have access to individuals’ private health information. Is that a need in order to enforce the provisions of the act?
Shulman: No. Absolutely not. What we will know is and ask for based on the law is: ‘Do you have health insurance coverage? If so, for how many months? And what is the name of the insurance company?’…
I think it’s been way overstated our role in health care. We are basically going to facilitate the financial transactions that make this whole law work. But we’re not going to have access to private individual health care information except for the fact of coverage.
Shulman said the IRS will match the information a taxpayer submits to what his or her insurer reports (see minute 9:00).
He also explained in a speech at the National Press Club in 2010 that taxpayers will attach a form to their tax return that insurers will send to them.
Shulman, April 5, 2010: When someone files their return, the insurance company will send us a little box that is checked, a yes-no question, that says, ‘Do they have coverage or not?’ They’ll send it to the individual. The individual will attach it to their return, and they’ll send it to us. Think it’s just like a 1099, where you get information reporting about the interest that you have on the bank account.
We will run matching programs around that. And if somebody doesn’t have coverage, they’ll either have paid the penalty that they owe, or they’ll get a letter [from] us saying that you owe this amount.
The IRS hasn’t officially announced procedures for how taxpayers will prove they have insurance. None is listed on the IRS’s web page dedicated to Affordable Care Act tax provisions. But the IRS proposed in April the types of information insurers must submit to the IRS in 2015 — and they don’t include personal health details.
The agency proposed asking insurers for the following:
- The name, address and Social Security Number or Tax Identification Number of the taxpayer and any dependents.
- Dates the insurer provided coverage.
- Whether the insurance is considered “qualified” under the law, which means it covers a number of broadly defined health benefits, among other requirements.
- Whether the individual bought insurance through an affordable insurance marketplace, known as a health insurance exchange.
- Whether the individual is eligible for tax credits and other assistance to help pay for coverage.
Abortion Coverage Required?
ATR claims employers must offer preventative coverage that includes “abortion and hair loss treatment.” That’s not true.
The law requires preventative coverage in insurance plans sold to small businesses and individuals. But the states define what that coverage is.
Some states already have laws banning abortion coverage — although some extend exemptions in cases of rape, incest or to save the life of the mother. Others states have chosen to include voluntary abortion coverage in plans offered to small businesses and individuals. But even then, the health care law requires those states to offer an additional plan that does not cover abortion.
ATR’s tax form asks taxpayers if their employer offers “affordable qualifying coverage.” And the instructions for this question claim that a qualified plan “must include necessary preventative coverage such as contraception, abortion, and hair loss treatment.”
It’s true the ACA specifically requires most health insurance plans to pay for contraception for women, coverage that at least 26 states mandated to some extent before the health care law. And it’s true the law includes new coverage requirements for preventative services. But those requirements apply to new insurance plans sold to individuals and small businesses that have 50 or fewer employees. The requirements do not apply to large employers, which make up about 70 percent of the insurance market.
The act’s intent is to make coverage sold to individuals and small businesses as comprehensive as typical employer-based plans. So, the law requires the smaller plans to cover 10 broadly defined “essential health benefits,” one of which is “preventative and wellness services.”
The ACA allows the states to define what those preventative services are in “benchmark” insurance plans.
The benchmark plans in Kansas, Kentucky and Utah, for example, do not cover voluntary abortion beyond at least one of the exceptions for rape, incest or to save the mother’s life. In fact, those states — and five others — outlawed private and public insurance from covering voluntary abortions before the ACA became law.
And 20 states have banned insurers from covering abortion in plans sold on exchanges, the affordable insurance marketplaces that states and/or the federal government are supposed to set up under the health care law.
States including California, Colorado and New York have picked benchmark plans that cover “voluntary” or “elective” abortions.
California’s plan, for example, requires a $30 copay for a “voluntary termination of pregnancy.”
But as we’ve written before, the law requires that at least one plan sold on a state exchange not include abortion coverage beyond the standard exceptions. (The law also bars federal subsidies from directly paying for a voluntary abortion.)
None of the benchmark plans in the six states mentioned above covers cosmetic hair loss treatment.
No Liens or Levies
The form also claims that “failing to comply with the Obamacare Tax Mandate could result … in interest against your personal property.” That’s not true.
As we’ve written before, the IRS cannot file a tax lien (a legal claim against such things as homes, cars, wages and bank accounts) or a levy (seizure of property or bank accounts).
The law specifically states on page 151 that the government cannot “file notice of lien with respect to any property of a taxpayer by reason of any failure to pay the penalty imposed by this section, or … levy on any such property with respect to such failure.’’
But as we noted, the law leaves room for the IRS to issue penalties and to sue to recover the unpaid tax, just as it does now for overdue taxes.
Waiver Whopper
The form’s instructions page also claims that taxpayers “can apply to the Secretary of the Department of Health and Human Services for a waiver from Obamacare.”
We’ve addressed similar claims before. The fact is HHS gave temporary waivers to companies — not individual taxpayers — pertaining to one provision of the law.
The health care law will gradually eliminate the annual and lifetime dollar limits placed on insurance benefits. The law raises the limits each year until 2014, when health plans can no longer place a cap on benefits.
HHS has granted waivers to more than 1,200 companies, particularly restaurants with low-income and part-time employees. The waivers allowed companies such as McDonald’s to temporarily continue to provide bare-bones insurance coverage to some workers.
The waivers, which affect nearly 4 million people, expire in 2014.
— Ben Finley