Editor’s note, May 17, 2023: The J&J vaccine is no longer available in the United States.
Quick Summary
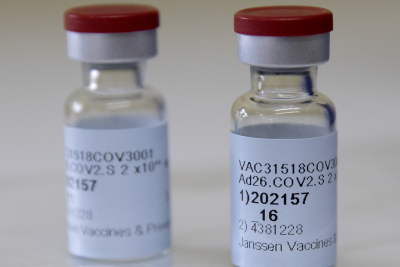
Vaccine name: Ad26.COV2.S
Design type: Adenovirus viral vector
Dose number: 1 dose, with a “booster” dose recommended for all adults at least two months later. At least two months after getting either 1 or 2 doses of the J&J vaccine, adults should get 1 bivalent mRNA shot, the CDC recommends.
Efficacy: Overall, 66.1% efficacy in preventing moderate to severe COVID-19 in adults 28 days or more after vaccination, but efficacy was higher in the U.S. population (72% efficacy in preventing moderate to severe COVID-19 and 85.9% efficacy in preventing severe or critical COVID-19) than in South Africa (64% and 81.7% efficacy in preventing moderate to severe or severe/critical disease, respectively), where the beta strain of coronavirus emerged.
Safety: In rare instances, the J&J vaccine likely causes a dangerous blood clotting condition combined with low blood platelets known as thrombosis with thrombocytopenia syndrome, or TTS. As of April 7, 2022, the syndrome has been confirmed in 60 cases, including nine deaths, after more than 18.6 million doses of the J&J vaccine. Although TTS remains rare, the FDA on May 5, 2022, limited authorized use to adults who can only get the J&J vaccine, among available options, due to medical reasons or who will only elect to take the J&J vaccine. The vaccine has also been linked to rare cases of Guillain-Barré Syndrome, a disorder in which the immune system attacks nerve cells. No serious safety concerns were reported during clinical trials. The shot, however, did elicit temporary side effects in some recipients, including pain at the injection site, headache, fatigue, and muscle pain or ache.
Doses administered: A little over 19 million doses of the J&J vaccine were administered in the U.S. As of May 7, 2023, the vaccine isn’t available in this country.
Expected timeline: On Feb. 27, 2021, the FDA authorized the vaccine for emergency use in adults age 18 and older. On May 5, 2022, the FDA limited that authorization to adults for whom other authorized or approved vaccines are not “clinically appropriate” or accessible, and to those who will only choose to get the J&J vaccine for COVID-19.
Operation Warp Speed involvement: The U.S. government provided about $1 billion for clinical trials and vaccine development. It spent another $1 billion for vaccine manufacturing, contracting for 100 million doses with an option to purchase up to another 200 million.
Storage considerations: Normal refrigerator temperature (36°F to 46°F) for six months.
More than two months after its last COVID-19 vaccine authorization, the FDA authorized for emergency use a one-shot vaccine from Janssen Biotech Inc., a Johnson & Johnson pharmaceutical company, on Feb. 27, 2021.

Unlike the Pfizer/BioNTech and Moderna vaccines, which use an mRNA design, the Johnson & Johnson shot uses a harmless adenovirus — a type of virus that typically causes the common cold — modified with the genetic material for SARS-CoV-2 to trigger an immune response. The Johnson & Johnson vaccine has the advantage of being one shot, not two. It also can be stored at regular refrigeration temperatures for up to six months — much longer than either of the mRNA vaccines.
Johnson & Johnson submitted its request for emergency use authorization on Feb. 4, 2021. An external panel advising the FDA met on Feb. 26, 2021, and voted unanimously (22 to 0) that “based on the totality of scientific evidence available … the benefits of the Janssen COVID-19 Vaccine outweigh its risks for use in individuals 18 years of age and older.” The FDA then authorized the vaccine for emergency use the following day.
On Oct. 20, 2021, the FDA authorized a second booster dose for all adults, given at least two months after the first dose. As with the other COVID-19 vaccines, any of the authorized or approved vaccines can be given as a booster following a single-dose J&J vaccine.
Due to concerns about a rare but serious blood clotting disorder coupled with low levels of platelets, a committee advising the Centers for Disease Control and Prevention voted to recommend the two mRNA vaccines over the J&J vaccine on Dec. 16, 2021. The CDC endorsed the “clinical preference” for the other vaccines the same day, while emphasizing that the J&J vaccine will remain available and vaccination with any vaccine is better than going unvaccinated.
Several months later, on May 5, the FDA limited authorized use to adults who either couldn’t get one of the other authorized or approved COVID-19 vaccines because of medical or access reasons, or only wanted a J&J vaccine for protection against the disease. The FDA’s decision was based on an evaluation of the rare risk of TTS and the availability of other vaccines that haven’t shown a risk for the condition.
But as of May 7, 2023, all of the J&J vaccines the government still had in stock expired, so the vaccine “is no longer available in the U.S.,” the CDC said. The agency’s recommendation is that adults who got 1 or 2 doses of the J&J vaccine get 1 dose of a bivalent mRNA vaccine, either Moderna or Pfizer/BioNTech, two months or more after their last vaccine dose.
Johnson & Johnson Q&A
What is in the vaccine and how does it work?
The design is different from the mRNA vaccines authorized in December, but all of the vaccines fundamentally work in the same way: They trigger an immune response against the SARS-CoV-2 virus’s spike protein, which sits on the surface of the virus and is what the virus uses to enter cells.
The Johnson & Johnson vaccine uses another, harmless virus — adenovirus 26 — modified with DNA for the SARS-CoV-2 spike protein. Adenoviruses typically cause common-cold symptoms, and for the vaccine, the virus is also modified so it can’t replicate in the body.
The modified adenovirus enters human cells, which then read the genetic material and begin making the coronavirus spike protein. This triggers the immune system, generating protective antibodies and activating other immune cells known as T cells.
In other words, the vaccine doesn’t include the COVID-19 virus, but rather, genetic material that prompts the body to produce an immune response to SARS-CoV-2 so that the body will recognize and react to the actual coronavirus if needed.
Dr. William Schaffner, an infectious disease expert with the Vanderbilt University School of Medicine, summarized how the vaccine works to CNN. “So essentially it’s a sheep in wolf’s clothing, and when your immune system sees it, it responds to it and creates protection against it and in the future, against the real virus that causes Covid-19,” he said.
How was the vaccine developed?
Johnson & Johnson has experience working with adenovirus-based vaccines, and gained approval in Europe in July for an Ebola vaccine that uses this technology.
The company is also working on adenovirus-based vaccines for HIV and Zika.
In January 2020, when the sequence for SARS-CoV-2 became available, Johnson & Johnson collaborated with Harvard’s Beth Israel Deaconess Medical Center to test multiple COVID-19 vaccine candidates. At the end of March, researchers announced they had identified a lead candidate.
In July 2020, J&J launched a phase 1/2a randomized controlled trial in the U.S. and Belgium with 1,051 participants ages 18 to 55 and over 65 to assess dosage, safety and immune response.
After the phase 1/2a trial showed a single dose of the vaccine produced neutralizing antibodies for COVID-19, J&J launched a phase 3 randomized controlled trial of a single dose. It began enrollment in the U.S. on Sept. 21, ultimately enrolling 44,325 people age 18 or older in the U.S., South Africa and six Latin American countries. Enrollment in that trial was complete on Dec. 17. The EUA application is based on the results of that trial, which is ongoing. Participants will be followed for two years.
J&J is also completing a second phase 3 randomized controlled trial in 10 countries, including the U.S., assessing a two-dose regimen. And it has started or is planning other clinical studies of its vaccine in children, pregnant women and their infants, and immunocompromised individuals.
How effective is the vaccine?
In its primary clinical trial, which was conducted in 2020 before the advent of the delta or omicron variants, J&J reported 66.1% efficacy globally in preventing moderate to severe COVID-19 in adults 28 days or more after vaccination, and an efficacy of 85.4% in preventing severe or critical COVID-19. The efficacy was similar across demographics including age, race and ethnicity.
Moderate to severe disease was defined as a positive COVID-19 test result and either one respiratory-related or deep vein thrombosis symptom, or two symptoms from a list including fever, chills, sore throat, cough, malaise, headache and gastrointestinal upset, the FDA said in its briefing document. A severe/critical case was defined as a positive test result and one symptom including clinical sign of severe systemic illness, respiratory failure, shock, admission to the ICU and death.
As we’ve explained before, a 66.1% efficacy roughly means a vaccinated person has a 66.1% reduced risk of developing moderate disease, compared with a similar person who wasn’t immunized.
Due to new variants of the virus emerging in the last few months of the trial, J&J provided data on efficacy by location, showing that the vaccine doesn’t appear to be as effective against the beta variant, which was first observed in South Africa.
In the U.S. population, there was 72% efficacy in preventing moderate to severe COVID-19 and 85.9% efficacy in preventing severe or critical disease, while in South Africa, those figures were 64% and 81.7%, respectively.
In Brazil, where the gamma variant first emerged, efficacy was closer to that of the U.S. population: 68.1% in preventing moderate to severe disease.
The vaccine had 100% efficacy in preventing COVID-19 that would require medical intervention — meaning hospitalization, ICU admission, mechanical ventilation or a life support machine — 28 days or more after vaccination.
As of Feb. 5, 2021, there were no COVID-19-related deaths in the vaccinated group and seven COVID-19-related deaths in the placebo group, the FDA briefing document said.
The participants in the vaccinated group who developed moderate symptoms had “fewer and less severe symptoms” than those in the placebo group, J&J said. After 28 days post-vaccination, 66 people developed such symptoms in the vaccinated group, compared with 193 in the placebo group. For severe/critical cases, there were five in the vaccinated group and 34 in the placebo group.
In the months since the J&J vaccine was deployed, real-world effectiveness and other data has borne out that the vaccine provides durable protection and also works against the delta variant, although it appears to be generally less protective compared with the two mRNA vaccines.
In September 2021, J&J announced that an observational study looking at insurance claims in the U.S. showed that its single dose vaccine was 81% effective in preventing COVID-19 hospitalization — a result that did not change much over time, even after the delta variant predominated. The company also reported that a second “booster” dose of its vaccine increased neutralizing antibodies in people and raised protection against moderate to severe or critical COVID-19 to 94% in the U.S. and 75% globally.
There is limited data about how well the J&J vaccine works against the omicron variant, which was first recognized in southern Africa in November.
Based on the mutation profile of omicron, scientists expect the vaccine to be significantly less protective against omicron infection compared with previous variants, but to still afford some protection against serious disease. Given evidence that booster shots can restore some of the neutralizing antibody response, public health officials recommend that all adults who have received one dose of the J&J vaccine receive a booster dose — preferably of one of the mRNA vaccines — at least two months after the first shot to offset potential waning immunity and to protect against both omicron and delta.
On Dec. 30, 2021, J&J announced preliminary clinical trial results from South Africa that found a first booster dose of the J&J vaccine was 85% effective in preventing COVID-19 hospitalization during a time when the omicron variant was dominant.
A subsequent study in the U.S. found a lower level of protection against hospitalization, with a single J&J dose 31% effective and two doses 67% effective, based on hospitalizations in 10 states between December 2021 and March 2022. That compared with 78% for an initial J&J dose paired with an mRNA booster and 90% for three mRNA doses.
Citing the results of that study, the CDC said on March 29, 2022, that people who only received J&J shots could get a second booster of one of the mRNA vaccines. Immunocompromised people and those over 50 years old could also get a second mRNA booster.
How safe is the vaccine?
There were “no specific safety concerns” identified in the trial, the FDA briefing document said. Some of those receiving the vaccine did report side effects, including injection site pain, headache, fatigue and myalgia (muscle pain or ache), generally lasting a day or two post-vaccination. These side effects were more common in 18- to 59-year-old participants.
Among the 44,325 participants in the phase 3 trial, 21,895 received the COVID-19 vaccine and 21,888 were in the placebo group.
The FDA determined three non-fatal serious adverse events in the vaccinated group were likely related to the vaccine: a hypersensitivity reaction involving urticaria or hives, injection site pain unresponsive to over-the-counter pain medicine, and a case involving a few days of symptoms including “generalized malaise, weakness, myalgia, shortness of breath, headache, sensation of numbness and tingling in upper extremities, chest pain and fever.”
The FDA noted two reports of Bell’s palsy, a form of temporary facial paralysis, in the vaccine group and two in the placebo group, and one case of Guillain-Barre Syndrome in each group. The FDA said those reports “are unlikely related to study vaccine but a causal relationship cannot be definitively excluded.”
Six vaccine recipients reported deep vein thrombosis, while two placebo recipients did so. Four vaccine recipients reported pulmonary embolism, as did one person in the placebo group. The FDA said there were risk factors among those individuals, but the imbalance between the vaccine and placebo groups meant that “vaccine cannot be excluded as a contributing factor,” recommending surveillance as the vaccine was deployed in larger populations.
There were also more reports of tinnitus, or ringing in the ears, among vaccine recipients: Six reports, compared with none in the placebo group. The FDA again said there was insufficient data to determine a causal relationship to the vaccine, complicated by the fact the individuals had risk factors.
And there were a few cases urticaria, or hives — eight in the vaccine group, three in the placebo group — which the FDA said are “possibly related” to the vaccine.
There were no reports of anaphylaxis immediately after vaccination; however, on Feb. 26, Johnson & Johnson said it had received a report of one such reaction in South Africa.
In late April 2021, the CDC and the FDA added fact sheets for the J&J vaccine about a suggested increased risk of rare blood clots combined with low levels of blood platelets, a dangerous condition called thrombosis with thrombocytopenia syndrome. The agencies had recommended a temporary 10-day pause in the use of the vaccine and investigated 15 cases of the rare condition among women, including three deaths, out of nearly 8 million vaccinations, as of April 21, 2021. For more information on the hiatus, see “Q&A on the Rare Clotting Events That Caused the J&J Pause.”
The CDC said of the J&J vaccine that “women younger than 50 years old especially should be aware of the rare risk of blood clots with low platelets after vaccination, and that other COVID-19 vaccines are available where this risk has not been seen.”
On Dec. 16, 2021, an advisory committee to the CDC reviewed the latest data on TTS, finding a slightly higher rate of cases and deaths than previously known. While TTS remains extremely rare overall, the reporting rate in females 30 to 49 years of age has been as high as about 1 in 100,000. In that highest-risk group, 2 females have died per million doses. The FDA has also noted that cases have occurred in adults of varying ages and in males. Additionally, the proportion of TTS cases leading to death did not decline after the J&J pause, when regulators had hoped sharing information about how best to treat the condition would cut down on the worst outcomes.
Given the availability of the mRNA vaccines, which have not been linked to TTS, the committee voted to preferentially recommend the Pfizer/BioNTech and Moderna vaccines. The CDC then endorsed that recommendation.
As of April 7, 2022, the agencies have confirmed 60 cases, including nine deaths, among more than 18.6 million J&J vaccines administered. That’s a reported case rate of 3.23 per million doses of vaccine given and a reported death rate of 0.48 per million doses.
On May 5, the FDA limited authorized use of the vaccine to adults who either couldn’t get one of the other authorized or approved COVID-19 vaccines because of medical or access reasons, or only wanted a J&J vaccine for protection against the disease.
While the overall risk of TTS is low, the FDA said it’s unknown what would put someone at risk for TTS after getting a J&J vaccine. That factor, along with the seriousness of the condition and the availability of other COVID-19 vaccines that haven’t demonstrated a risk for TTS, led to the FDA’s decision to limit authorized use.
“Today’s action demonstrates the robustness of our safety surveillance systems and our commitment to ensuring that science and data guide our decisions. We’ve been closely monitoring the Janssen COVID-19 Vaccine and occurrence of TTS following its administration and have used updated information from our safety surveillance systems to revise the EUA,” Dr. Peter Marks, director of the FDA’s Center for Biologics Evaluation and Research, said in a press release.
On July 13, 2021, the FDA added warnings to fact sheets on the vaccine about an observed increased risk of the neurological disorder Guillain-Barré Syndrome.
The agency said the chance of developing the syndrome is “very low” but advised J&J vaccine recipients to seek medical attention if they experience symptoms including weakness or tingling, particularly in the legs or arms; difficulty walking or with facial movement; double vision; or bladder control or bowel function issues.
The warning came after preliminary reports of 100 cases, with most people reporting symptoms within 42 days of vaccination. One death was reported, but it isn’t known whether the death or the cases were caused by the vaccine.
“Although the available evidence suggests an association between the Janssen vaccine and increased risk of GBS, it is insufficient to establish a causal relationship,” the FDA said. About 3,000 to 6,000 people each year in the U.S. develop the syndrome, in which nerve cells are damaged by the immune system, leading to weakness and even paralysis, according to the FDA. The agency said that most recover fully.
As of April 7, 2022, there had been about 313 preliminary reports of GBS. Most cases occurred around two weeks post-vaccination and in males, primarily those 50 years of age and older.
Other work has further supported a link between the J&J vaccine and GBS. A 2024 report from the National Academies of Sciences, Engineering, and Medicine concluded that the evidence “favors acceptance of a causal relationship” between the vaccine and GBS, as well as TTS.
Editor’s note: This story will be updated as necessary.
Editor’s note: SciCheck’s COVID-19/Vaccination Project is made possible by a grant from the Robert Wood Johnson Foundation. The foundation has no control over our editorial decisions, and the views expressed in our articles do not necessarily reflect the views of the foundation. The goal of the project is to increase exposure to accurate information about COVID-19 and vaccines, while decreasing the impact of misinformation.